Influenza (FLU) Update for Week Ending 12-22-18
For week #51 (ending 12-22-18) the CDC reported that influenza (Flu) activity, which includes diagnosed flu as well as ILI (Influenza-Like-Illness) continued to increase. The percentage of respiratory specimens testing positive for flu increased to 15.6% from 11.0% last week.
Influenza A viruses are the most common found in sample testing, with Influenza A(H1N1)pdm09 the most dominant, except for Region 4 (the Southeast), which again had A(H3N2) dominate. Influenzas A (H1N1), A (H2N2) and Influenza B viruses tested were considered to be co-circulating. Also, the majority of the flu viruses were genetically similar with the 2018/19 Flu Vaccine.
FirstWatch RIN (Regional Influenza Network) Alerts increased again last week over the previous week.
For the recently reported week ending December 22, 2018, the CDC reported: Influenza-like illness (ILI) visits to clinics & other non-hospital facilities was 3.3% (l. w. 2.7%) & is above the national baseline of 2.2%. Nine (9) of the 10 regions (all except Region10) reported ILI at or above their region-specific baselines; it was 8 of 10 Regions last week. New York City and nine (9) states had high ILI activity, Puerto Rico and seven (7) states had moderate ILI activity; and 11 states reported low levels; and Washington DC and 22 states had minimal ILI activity, and one (1) state reported insufficient data.
Flu cases indicating spread (documented by positive flu tests on respiratory specimens) were reported as Widespread in Guam and 11 states; Regional in Puerto Rico and 19 states; 15 states reported local activity; Washington DC, the US Virgin Islands and three (3) states reported sporadic flu activity. Clinical lab testing for influenza was positive for 15.6% of specimens, compared to 11% last week, with a range of 4.9% (Region 10) to 19.9% in Region 4 (the only region with A (H3N2) as the dominant strain.
Influenza A remained the dominant flu for 96.7% of the flu tests reported (94.6% last week), with 89.2% (81.9% last week) as A (H1N1) pdm09 viruses and the H3N2 subtype at 10.8% (18.1% last week). The rest of the tests showed 3.3% (5.4% l.w.) tested as Influenza B viruses, with 14.3% (42.9% l.w) of Yamagata lineage and 85.7% (57.1% l.w.) Victoria lineage.
This shows a small increase in Influenza A viruses and therefore slightly less Influenza B. Typically, Influenza B viruses cause less severe illness and occur more towards the Spring.
All the flu viruses that were tested were susceptible to the antivirals oseltamivir, zanamivir, and peramivir (Tamiflu, Relenza, and Rapivab, respectively). There was high resistance to the adamantane group of antivirals, namely Amantadine and rimantadine (Flumadine), which are not effective for any Influenza B viruses). Baloxavir marboxil, under the brand name Xofluza, is a new influenza antiviral drug approved in October, 2018, as a new alternative. It also works on Influenza B viruses and controls the virus in a different way.
The CDC recommends as early as possible treatment with antivirals for those confirmed or suspected flu with severe, complicated, or progressive disease, who are hospitalized, or at high risk for complications of flu. See this link for a list of those at risk for complications from flu: https://www.cdc.gov/flu/about/disease/high_risk.htm
The CDC provides an interactive U.S. map that will link to each state’s public health authorities. ILI and Flu information and processes, as well as other diseases and public health topics. This site includes a tremendous amount of information at the State and even Local level.
Find it at this site: https://www.cdc.gov/flu/weekly/usmap.htm
For Influenza-Like Illness:
High ILI Activity: (New York City & 9 states):
Alabama, Colorado, Georgia, Kentucky, Louisiana, Maryland, New Jersey, New Mexico, and South Carolina
Moderate ILI Activity: (Puerto Rico & 7 states):
Arizona, Arkansas, Indiana, Mississippi, Oklahoma, Utah, and Virginia
Low Activity: (11 states):
California, Illinois, Massachusetts, Minnesota, Missouri, Nevada, New York, North Carolina, Pennsylvania, Texas, and Wisconsin
Minimal Activity: (Washington D.C. & 22 states):
Connecticut, Delaware, Florida, Hawaii, Idaho, Iowa, Kansas, Maine, Michigan, Montana, Nebraska, New Hampshire, North Dakota, Ohio, Oregon, Rhode Island, South Dakota, Tennessee, Vermont, Washington, West Virginia, and Wyoming
Insufficient Data: Alaska
For Flu (positive flu tests):
Widespread Activity: (Guam & 11 states):
Arizona, California, Connecticut, Delaware, Florida, Georgia, Massachusetts, Nebraska, New Mexico, New York, and North Carolina,
Regional Activity (Puerto Rico & 19 states): Alabama, Colorado, Idaho, Illinois, Indiana, Kentucky, Louisiana, Montana, Nevada, New Hampshire, New Jersey, Ohio, Oklahoma, Pennsylvania, Rhode Island, South Carolina, Texas, Utah, and Vermont,
Local Activity (15 states): Arkansas, Iowa, Kansas, Michigan, Minnesota, Mississippi, Missouri, North Dakota, Oregon, South Dakota, Virginia, Washington, West Virginia, Wisconsin, and Wyoming
Sporadic Activity: (Washington D.C., U.S. Virgin Islands, & 3 states): Alaska, Hawaii, and Maine
States Did Not Report: (2 states): Maryland and Tennessee
Other Data:
The Hospitalization rate from Flu was 3.6 per 100,000 (last week 2.9%). Children (ages 0-4) had the highest hospitalization rate of 10.0 per 100,000 (last week 7.7%), with older adults (age > 65 years) at 8.0% per 100,000 (l.w. 6.6%); and adults (age 50-64 years) at 4.1% per 100,000 (l.w. 3.4%). Most, 86.5% (l.w. 84.0%), were caused by Influenza A viruses; 11.9% (l.w. 13.8%) were from Influenza B viruses; 1.1% (l.w. 1.3%) showed co-infection with both Influenza A and B viruses; and 0.4% (l.w. 1.0%) were not typed for a specific flu virus.
Death rates for pneumonia and influenza in adults (6.2%) is below the epidemic threshold of 6.8% for week #50. Death reports often aren’t reported for data purposes the same week.
There were four (4) pediatric deaths attributed to flu reported this week, for a total of 11 for this flu season
Flu in Canada, Europe & the World:
Canada:
A Flu Summary was not posted for week ending 12/22/18. A report on Jan 4, 2019 will include both Weeks 51 & 52.
For more specific information see:
On flu activity:
https://www.canada.ca/en/public-health/services/publications/diseases-conditions/fluwatch/2018-2019/week50-december-9-december-15-2018.html
Canadian Flu Information:
https://www.canada.ca/en/public-health/services/diseases/flu-influenza.html
General Page for Canadian Flu Watch Surveillance with links to different components:
https://www.canada.ca/en/public-health/services/diseases/flu-influenza/influenza-surveillance.html
About the Canadian Influenza Activity Surveillance System:
https://www.canada.ca/en/public-health/services/diseases/flu-influenza/influenza-surveillance/about-fluwatch.html
Europe:
According to the European Center for Disease Prevention & Control (ECDC), for week 12/17 to 12/23/18, only 28 of 51 countries reported. Influenza activity was at baseline or low levels throughout the European Region, but continues to increase. The majority of circulating virus remained Influenza A for patients both in hospital and out; 21.8% of tested specimens were positive for flu.
For more information see: https://flunewseurope.org/
World:
The World Health Organization (WHO) provides info on Influenza in Member Countries here: https://www.who.int/influenza/surveillance_monitoring/en/
First Responder Specific Information
There are many websites that may be helpful in planning and managing seasonal flu within First Responder organizations. A few of those websites are included here:
NIOSH on Flu for Employers/Employees:
https://www.cdc.gov/niosh/topics/flu/
Protection from Flu:
https://www.cdc.gov/flu/protect/habits/index.htm
Weekly Flu Map:
https://www.cdc.gov/flu/weekly/usmap.htm
World Map Showing Flu & Other Infectious Diseases:
https://www.healthmap.org/en/
Other Actions First Responders Should Consider
- First Responders should be vaccinated for Flu each season to prevent getting flu themselves, taking it home to family members, or transmitting it to patients in their care. Family members and patients may be at increased risk of complications from flu.
- Perform proper hand hygiene including frequent handwashing and the use of hand sanitizers in general, and particularly when providing patient care or after touching surfaces.
- Masks (N95 or N100) should be used in the presence of patients with cough and/or fever; preferably before being within 6 feet of the patient. This becomes even more important if droplet producing procedures are being performed (i.e. suctioning, nebulizer treatments, BVM, intubation).
- Care should be taken to avoid touching your own face and mucous membranes (eyes, mouth, nose) since the flu virus is frequently found on surfaces such as door knobs, writing & recording tools (pens and tablets), cot and equipment handles, phones, light switches, as well as clothing, bed clothes, etc.
- Report signs/symptoms of flu to your physician or other appropriate provider for early assessment and care. Alert your employer per policy.
- Cough and sneeze into your sleeve, if a tissue is not available, and not onto your hands. Watch this Youtube video for a humorous but educational approach on the subject. https://www.youtube.com/watch?v=CtnEwvUWDo0
- Stay away from others if you are sick.
- Be aware of your exposure risk and history to prevent exposing others. Take extra precautions or avoid those with immunocompromise, when possible, if you have a known or likely exposure.
- Antivirals may be indicated for the treatment of flu, particularly for those in high risk groups, those who are hospitalized or have severe, complicated or progressing flu. Those that present with 48 hours of the onset of symptoms may also be given antivirals, based on PCP judgement but make sure the practitioner is aware of their Frist Responder Role. See https://www.cdc.gov/flu/antivirals/whatyoushould.htm
And, for consideration when looking at yourself, your family and friends, or your patients, consider the following information regarding complications of flu:
Flu is much more worrisome for the very young and the elderly, as well as those who fit into one of the high risk categories see this link for the list: https://www.cdc.gov/flu/about/disease/high_risk.htm . Signs of ILI/Flu in this group requires careful assessment to rule out complications and these groups are much more likely to need medical oversight to assure adequate care. Young children and those over 65 are typically at greater risk for complications, hospitalization, and even death.
Consideration should be given to perhaps monitoring these groups more closely, with inclination for more comprehensive assessment and transport for further evaluation, when presented with possible flu and any signs of complications.
Complications of flu, sometimes requiring hospitalization and even leading to death, tend to occur after the person has begun to get better from the flu and then appears to relapse. EMS personnel may want to look more closely at those patients when the call is not about the initial signs and symptoms of flu, but about increasing or different signs that have appeared, often from five days to two weeks after the initial flu symptoms began.
A study was published by the Institute for Clinical Evaluative Sciences in NEJM (New England Journal of Medicine). See details below:
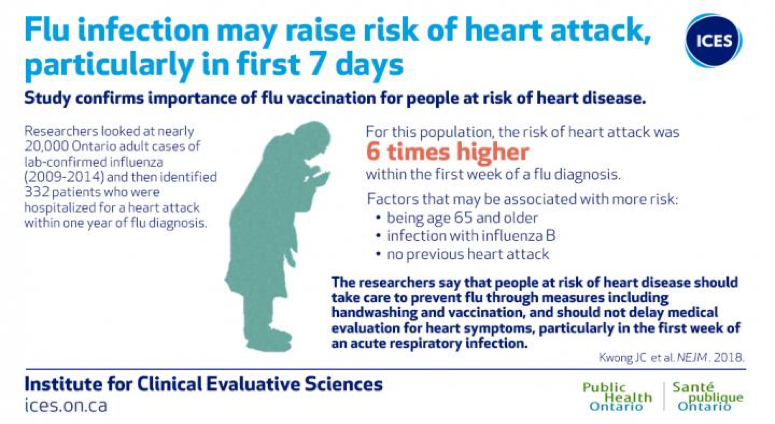
Image courtesy of ICES/PHO
“The researchers add that patients should not delay medical evaluation for heart symptoms particularly within the first week of an acute respiratory infection.” (Lisa Schnirring, News Editor: CIDRAP News ;Jan 25, 2018)
For more information on Influenza and the Heart Attack Study, please see the link below.
https://www.eurekalert.org/pub_releases/2018-01/pho-rcl011818.php

