Influenza (FLU) Update for Week Ending 12-28-19
Influenza (FLU) Update for Week #52 — Week Ending 12-28-19
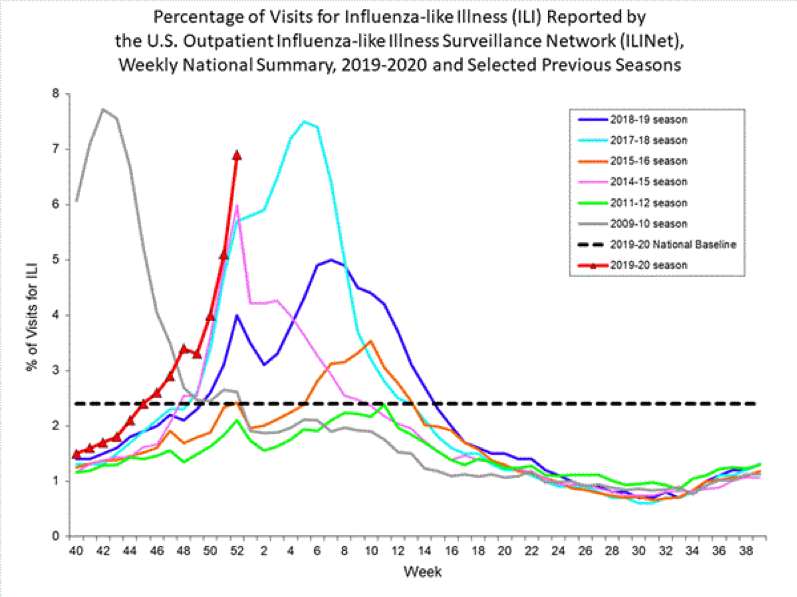
The CDC reported that flu activity (diagnosed flu and ILI outpatient visits) is high in all regions of the US and is continuing to increase. It has been elevated for eight (8) weeks now, longer at this time point than in most previous seasons. It is also important to note that Flu/ILI might be underreported for this time period because of the holidays and less people going for outpatient/doctor office visits. The complication rate may also be higher, when compared to other reporting periods, since the number of those diagnosed with flu may be skewed lower and show a higher rate of complications in comparison to the overall number diagnosed, since those with complications are more likely to have to seek medical care. The chart below is displaying the number of ILI cases reported by ILINet for this flu season, as well as other specific recent ones, for comparison. Please note that the only year that shows an earlier start than this year (the red line) is the year of the 2009/10 Pandemic Flu (the silver line). Also of interest is how early this season crosses the national baseline compared to other seasons, and how almost straight up the trajectory is with no sense that the cases will level off any time soon. The hope has to be that we don’t combine the case rates seen during the 2009/10 (silver) and 2017/18 (aqua) seasons with the extraordinary and record setting length of last year’s season (purple).
Nationally, most of the current flu activity is caused by Influenza B/Victoria which typically occurs in late Winter or Spring, nearer the end of the flu season, and often seems to hit the pediatric population particularly hard. A(H1N1) comes in next, with A(H3N2) and B/Yamagata circulating with much lower levels of flu. The predominant flu virus varies by both age and region.
The CDC estimated that at this point in the season, there have been at least 6.4 million sick with flu, 55,000 hospitalizations, and 2,900 deaths. Influenza-like illness (ILI) is defined as a temperature at/above 100o F [37.8o C] and cough and/or sore throat without a known cause other than flu. A Flu case, that is included in CDC data, indicates a positive flu test read by either a Clinical or Public Health Lab.
Diagnosed Flu and ILI are expected to continue to increase over the next few weeks and flu activity is likely to persist for several more months. It is recommended by public health officials & health care providers, that for all those 6 months or older, flu vaccinations be completed ASAP unless there is a valid medical contraindication. Most will receive a vaccination that covers 4 strains of influenza. See this link for more details, including charts, graphs, and maps: https://www.cdc.gov/flu/weekly/index.htm
FirstWatch RIN (Reginal Influenza Network) Alerts occurred frequently.
For the most recently reported week ending December 28, 2019, the CDC reported:
–ILI visits to clinics and other non-hospital facilities was at 6.9% and above the national baseline of 2.4%. The regional range was between 3.8% and 13.9% for Week #52. All ten regions reported that outpatient visits for ILI were at/above their own regional baselines.
–Flu cases, documented by positive flu tests from Clinical Labs, showed that 26.3% of respiratory specimens tested for influenza were positive, which is higher than last week’s report of 23%.
–Clinical Labs, which test many specimens to determine whether flu cases are increasing, decreasing, or staying stable, as well as a simple breakdown of A and B flu percentages, reported that of the 26.3% positive flu specimens, 67.9% were influenza B and 32.1% influenza A.
–Public Health Labs report data using a more limited number of specimens but provide a more specific breakdown of specific flu virus strains. Influenza B was detected at 59.6% and Influenza A at 40.4%. Further breakdown revealed that Influenza B showed 99.6% Victoria lineage and 0.4% Yamagata, while H1N1 is the dominant A with 91.3% with H3N2 at 8.7%.
Nationally, B/Victoria is the most common flu virus reported in children ages 0-4 years (48% of reported viruses) and ages 5-24 years (59% of reported viruses), while A(H1N1)pdm09 is the most common flu virus in ages 25-64 (42% of reported viruses) and those ages 65 and older (43% of reported viruses). Influenza B virus strains can be particularly hard on children.
To access specific state and regional information on circulating flu viruses, please see: https://gis.cdc.gov/grasp/fluview/fluportaldashboard.html
–Antiviral Resistance: At this time, >99% of the flu samples are susceptible to the four antivirals currently marketed for flu. This is particularly important for those at increased risk for complications from flu or with signs of severe flu. It is also important to start the antiviral as soon as flu symptoms appear. Consult your Health Care Provider to see if antivirals might be appropriate for you or someone in your family.
–Vaccine Coverage: Testing of influenza A(H1N1)pdm09 samples revealed that all samples tested were well matched with the components in the 2019-20 flu vaccine, while only 34.1% of the the A(H3N2) influenza virus samples were matched; 58% of B/Victoria virus samples were a similar match but B/Yamagata samples matched 100%. Unfortunately, it is the B/Victoria that is currently dominant nationally although specific areas or regions may differ. A more comprehensive report on vaccine effectiveness will be posted by the CDC at a later date and will provide a more complete picture of vaccine coverage of this year circulating flu strains.
The CDC provides an interactive U.S. map that will link to each state’s public health authorities, ILI and Flu information and processes, as well as other diseases and public health topics. This site includes a tremendous amount of information at the State, and even Local, level.
Find it at this site: https://www.cdc.gov/flu/weekly/usmap.htm
—For Influenza-Like Illness (ILI)
High ILI Activity (Washington D.C., New York City, Puerto Rico & 34 states): Alabama, Alaska, Arizona, Arkansas, California, Colorado, Connecticut, Georgia, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maryland, Massachusetts, Mississippi, Nebraska, New Jersey, New Mexico, New York, North Carolina, North Dakota, Oklahoma, Oregon, Pennsylvania, South Carolina, Tennessee, Texas, Utah, Virginia, Washington, West Virginia, and Wisconsin,
Moderate ILI Activity (9 states): Florida, Maine, Minnesota, New Hampshire, Ohio, Rhode Island, South Dakota, Vermont, and Wyoming
Low Activity (5 states): Hawaii, Michigan, Missouri, Montana, and Nevada
Minimal Activity (2 states): Delaware and Idaho
Insufficient Data to Calculate: U.S. Virgin Islands
—For Flu (positive Flu tests)
Widespread Activity (Puerto Rico & 45 states): Alaska, Alabama, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Idaho, Illinois, Indiana, Iowa, Kentucky, Louisiana, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Carolina, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, Washington, West Virginia, Wisconsin, and Wyoming
Regional Activity (4 states): Kansas, Maine, North Dakota, and Vermont
Local Activity (Washington D.C., & 1 state): Hawaii
Sporadic Activity: (U.S. Virgin Islands & 0 states)
No Activity: (0 states)
No Report: Guam
—Other Data:
Hospitalizations from Flu: The hospitalization rates have doubled, or nearly doubled, from just a couple of weeks prior to this current report. Specifically, there were a total of 2,667 lab-confirmed influenza-related cases that were reported hospitalized between 10/1/19 and 12/28/19. The hospitalization rate for all ages increased to 9.2 per 100,000. The highest rate was in those aged > 65 years (19.9/100,000), then children ages 0-4 (17.8/100,000), and then adults ages 50-64 (10/100,000). A slight majority were from infections with influenza A (51.5%), 47.8% with influenza B, 0.4% with both influenza A and B co-infection, and 0.3% which did not have a flu type determined. For the influenza A positives that had subtyping performed, 80.7% were A(H1N1); only 19.3% were A(H3N2).
Death rates for pneumonia & influenza in adults: from data as of 1/2/20, 5.5% of adult deaths during week #51 (ending 12/21) were associated with influenza and pneumonia. This is below the epidemic threshold of 6.8% for that week. This data reporting typically lags a week or more behind the reporting week and data may be even slower than normal because of the holidays.
Five (5) pediatric deaths associated with influenza were reported during week #52 but occurred in weeks #50 and #51. Two (2) of the cases were influenza B and only two had lineage tested with both those being B/Victoria; three (3) were typed as influenza A. A total of 27 pediatric deaths can be attributed to influenza for the 2019-20 Season. Eighteen (18) of them were from influenza B viruses, with all five (5) of the ones with determined lineage, B/Victoria. Nine (9) of the deaths were from influenza A viruses; the four (4) that had subtyping were all A(H1N1)pdm09 viruses.
International:
Canada:
Flu Reports in Canada for Weeks #51 & #52 were not published by PHAC plan. Reports pick back up again 1/10/20. However, according to the Public Health Agency of Canada (PHAC) Respiratory Virus report, the graphs looked at from a national perspective indicate that influenza activity continued to increase with about an equal amount of influenza A and B. Individual Provinces and Territories may present a different picture. For more specific information use this link:
https://www.canada.ca/en/public-health/services/surveillance/respiratory-virus-detections-canada.html
PHAC Home Page for Surveillance on Flu: https://www.phac-aspc.gc.ca/fluwatch/
Public Health Agency of Canada (PHAC) Home Page for Information on Flu:
https://www.canada.ca/en/public-health/services/diseases/flu-influenza.html
PHAC Provides Flu Watch Summary & Link to Full Influenza Reports Past & Present:
https://www.canada.ca/en/public-health/services/diseases/flu-influenza/influenza-surveillance/weekly-influenza-reports.html
PHAC Interactive Map for Flu Activity Across Canada:
https://www.canada.ca/en/public-health/services/diseases/flu-influenza/influenza-surveillance/map-activity-levels.html
Europe:
European Center for Disease Prevention & Control – Flu for Week #52 (12/23 – 12/29, 2019):
Although not all Member States (countries) reported, Influenza activity continued to increase across Europe with some countries reporting increased intensity and spread, although most still reported rates at or below baseline. For the sixth week in a row, specimens tested positive for flu, for those going to sentinel PCPs for ILI and ARI, at greater than 10%. The majority of flu cases were from Influenza A (62%), a decrease from 75% in Week #50, although a number of countries reported more cases of influenza B, or a mixed dominance of both A and B.
For more info see: https://flunewseurope.org/
Public Health England Flu Summary:
https://www.gov.uk/government/statistics/weekly-national-flu-reports
Global:
World Health Organization (WHO) Weekly Flu Summary (FluNet):
https://www.who.int/influenza/gisrs_laboratory/flunet/en/
WHO Global Flu Overview with Map and Text:
https://www.who.int/influenza/surveillance_monitoring/updates/latest_update_GIP_surveillance/en/
Global Epidemiology Reports:
WHO Collaborating Centers for Flu in Australia, Japan, & the United Kingdom
First Responder Specific Information
There are many websites that may be helpful in planning and managing seasonal flu within First Responder organizations. A few of those websites are included here:
NIOSH on Flu for Employers/Employees:
https://www.cdc.gov/niosh/topics/flu/
NIOSH Listing on Absenteeism in the Workplace throughout the US:
https://www.cdc.gov/niosh/topics/absences/default.html
Protection from Flu:
https://www.cdc.gov/flu/protect/habits/index.htm
World Map Showing Flu & Other Infectious Diseases:
https://www.healthmap.org/en/
- First Responders should be vaccinated for Flu each season to prevent getting flu themselves, taking it home to family members or transmitting it to patients in their care. Family members and patients may be at increased risk of complications from flu.
- Perform proper hand hygiene including frequent handwashing with soap and water, and the use of hand sanitizers in general, and particularly when providing patient care or after touching surfaces.
- Masks (N95 or 100) should be used in the presence of patients with cough and/or fever. Procedure or surgical masks can also be used but may not provide the same level of protection.
- Care should be taken to avoid touching their own face and mucous membranes (eyes, mouth, nose) since the flu virus is frequently found on surfaces such as door knobs, cot and equipment handles, phones, as well as clothing, bed clothes, etc. Once picked up on the hands from touching inanimate objects or from the secretions of a patient, it can transmit the flu (or any respiratory infection virus) via the mucous membranes of the face and head.
- Report signs/symptoms of flu to your physician or other appropriate provider for early assessment and care. Signs & symptoms suggest a period of contagiousness and out your patients and co-workers at risk.
- Cough and sneeze into your sleeve, if a tissue is not available, and not onto your hands.
- Stay away from others if you are sick.
- Be aware of your exposure risk and history. Take extra precautions or avoid those with immunocompromise, when possible, if you have a known or likely exposure.
- Antivirals may be indicated for the treatment of flu, particularly for those in high risk groups, those who are hospitalized or have severe, complicated or progressing flu. Those that present with 48 hours of the onset of symptoms may also be given antivirals, based on PCP judgement but make sure the practitioner is aware of their Frist Responder Role. See https://www.cdc.gov/flu/antivirals/whatyoushould.htm
- Flu is much more worrisome for the very young and the very old. Signs of ILI in this group requires careful assessment to rule out complications and these groups are much more likely to need to be transported to assure adequate care. Young children and those over 65 are typically at greater risk for complications, hospitalization, and even death. Hospitalization rates may also be elevated in those aged 50-64. Consideration should perhaps be given to monitoring these groups more closely, with inclination for more comprehensive assessment and transport for further evaluation, when presented with possible flu and any signs of complications.
Complications of flu, sometimes requiring hospitalization and even leading to death, tend to occur after the person has begun to get better from the flu and then appears to relapse. EMS personnel may want to look more closely at those patients when the call is not about the initial signs and symptoms of flu, but about increasing or different signs that have appeared.
- A study was published by the Institute for Clinical Evaluative Sciences in NEJM:
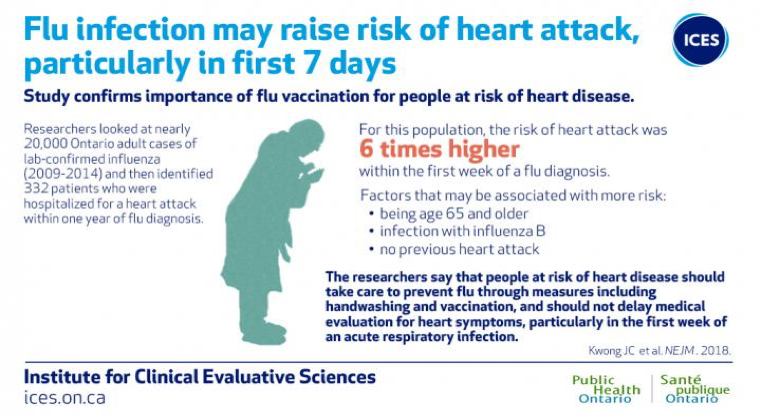
Image courtesy of ICES/PHO “The researchers add that patients should not delay medical evaluation for heart symptoms particularly within the first week of an acute respiratory infection.” (Lisa Schnirring, News Editor: CIDRAP News; Jan 25, 2018)
For more information on the Influenza and Heart Attack Study, please see the link below.
https://www.eurekalert.org/pub_releases/2018-01/pho-rcl011818.php


