Influenza (FLU) Update for Week Ending 12-29-18
For week #52 (ending 12-29-18) the CDC reported that influenza (Flu) activity, which includes diagnosed flu as well as ILI (Influenza-Like-Illness), continued to increase. The percentage of respiratory specimens testing positive for flu decreased to 13.7% from 15.6% last week, but all Regions were reporting flu levels above baseline and the number of cases of ILI and Flu continued to increase, as did hospitalizations.
Influenza A viruses are the most common found in sample testing, with Influenza A(H1N1)pdm09 the most dominant, except for Region 4 (the Southeast), which again had A(H3N2) dominate. Influenzas A (H1N1), A (H2N2) and Influenza B viruses tested were considered to be co-circulating. The majority of the flu viruses were genetically similar with the 2018/19 Flu Vaccine.
FirstWatch RIN (Regional Influenza Network) Alerts increased last week over the previous week.
For the recently reported week ending December 29, 2018, the CDC reported:
Influenza-like illness (ILI) visits to clinics & other non-hospital facilities was 4.1% (l. w. 3.3%) & is above the national baseline of 2.2%. For the first time this season, all 10 regions reported ILI at or above their region-specific baselines, although, like after Thanksgiving, the numbers may be a little skewed since less people usually go to health care providers for wellness care. New York City and 19 states had high ILI activity; nine (9) states had moderate ILI activity; Washington DC and 10 states reported low levels; and Puerto Rico and 12 states had minimal ILI activity.
Flu cases indicating spread (documented by positive flu tests on respiratory specimens) were reported as Widespread in 24 states; Regional in Puerto Rico and 18 states; six (6) states reported local activity; Washington DC, the US Virgin Islands and two (2) states reported sporadic flu activity; Guam did not report. Clinical lab testing for influenza was positive for 13.7% of specimens, compared to 15.6% last week, with a range of 6.5% (Region 3) to 19.5% in Region 4, the only region with A (H3N2) as the dominant strain.
Influenza A remained the dominant flu for 97.1% of the flu tests reported (96.7% last week), with 89.4% (89.2% last week) as A (H1N1)pdm09 viruses and the H3N2 subtype at 10.6% (10.8% last week). The rest of the tests showed 2.9% (3.3% l.w.) tested as Influenza B viruses, with 25% (14.3% l.w) of Yamagata lineage and 75% (85.7% l.w.) Victoria lineage.
This shows a small increase in Influenza A viruses and therefore slightly less Influenza B. Typically, Influenza B viruses cause less severe illness and occur more towards the Spring.
All the flu viruses that were tested were susceptible to the antivirals oseltamivir, zanamivir, and peramivir (Tamiflu, Relenza, and Rapivab, respectively). There was high resistance to the adamantane group of antivirals, namely Amantadine and rimantadine (Flumadine), which are not effective for any Influenza B viruses). Baloxavir marboxil, under the brand name Xofluza, is a new influenza antiviral drug approved in October, 2018, as a new alternative. It also works on Influenza B viruses and controls the virus in a different way.
The CDC recommends as early as possible treatment with antivirals for those confirmed or suspected flu with severe, complicated, or progressive disease, who are hospitalized, or at high risk for complications of flu. See this link for a list of those at risk for complications from flu: https://www.cdc.gov/flu/about/disease/high_risk.htm
The CDC provides an interactive U.S. map that will link to each state’s public health authorities. ILI and Flu information and processes, as well as other diseases and public health topics. This site includes a tremendous amount of information at the State and even Local level.
Find it at this site: https://www.cdc.gov/flu/weekly/usmap.htm
For Influenza-Like Illness:
High ILI Activity: (New York City & 19 states): Alabama, Arizona, Colorado, Georgia, Illinois, Indiana, Kansas, Kentucky, Louisiana, Massachusetts, Mississippi, Nevada, New Jersey, New Mexico, Oklahoma, South Carolina Texas, Utah, and Virginia
Moderate ILI Activity: (9 states): Arkansas, California, Michigan, Missouri, New York, North Carolina, Pennsylvania, Rhode Island, and Vermont
Low Activity: (Washington D.C. & 10 states): Connecticut, Florida, Iowa, Minnesota, Montana, Nebraska, Ohio, Oregon, Wisconsin, and Wyoming
Minimal Activity: (Puerto Rico & 12 states): Alaska, Delaware, Hawaii, Idaho, Maine, Maryland, New Hampshire, North Dakota, South Dakota, Tennessee, Washington, and West Virginia
For Flu (positive flu tests):
Widespread Activity: (24 states): Alabama, Arizona, California, Colorado, Connecticut, Delaware, Florida, Georgia, Idaho, Indiana, Kentucky, Louisiana, Massachusetts, Nebraska, New Jersey, New Mexico, New York, North Carolina, Pennsylvania, Rhode Island, South Carolina, Utah, Vermont, and Virginia
Regional Activity (Puerto Rico & 18 states): Arkansas, Illinois, Iowa, Kansas, Michigan, Missouri, Montana, Nevada, New Hampshire, North Dakota, Ohio, Oklahoma, Oregon, South Dakota, Tennessee, Texas, West Virginia, and Wyoming
Local Activity (6 states): Maine, Maryland, Minnesota, Mississippi, Washington, and Wisconsin
Sporadic Activity: (Washington D.C., U.S. Virgin Islands, & 2 states): Alaska, and Hawaii
Did Not Report: Guam
Other Data:
The Hospitalization rate from Flu was 5.4 per 100,000 (last week 3.6%). Children (ages 0-4) had the highest hospitalization rate of 14.5 per 100,000 (last week 10%), with older adults (age > 65 years) at 11.9% per 100,000 (l.w. 8%); and adults (age 50-64 years) at 6.2% per 100,000 (l.w. 4.1%). Most, 89.4% (l.w. 86.5%), were caused by Influenza A viruses; 9.3% (l.w. 11.9%) were from Influenza B viruses; 1.0% (l.w. 1.1%) showed co-infection with both Influenza A and B viruses; and 0.3% (l.w. 0.4%) were not typed for a specific flu virus.
Death rates for pneumonia and influenza in adults (6.1%) is below the epidemic threshold of 6.9% for week #51. Death reports often aren’t reported for data purposes the same week.
There were two (2) pediatric deaths attributed to flu reported this week, for a total of 13 for this flu season
Flu in Canada, Europe & the World:
Canada:
A Flu Summary was not posted for week ending 12/22/18. This report included both Weeks # 51 & 52.:
Flu activity increased and all indicators either increased or were similar to the previous week, with the tests positive 25.1% in Week # 51 and 29.4% in Week #52. Influenza A was the most common strain (99%); A (H1N1) (94%) caused the most cases. The majority of the confirmed flu cases and hospitalizations were for those under age 65. 68% of all Influenza A (H1N1)pdm09 cases were in those younger than 45 years old; 63% of all the Influenza A (H3N2) were reported in those 65 years and older.
Localized Activity by 7 Regions: Alta. (1), Ont. (4), B.C. (1), and N.B. (1)
Sporadic Activity by 31 Regions: B.C. (4), Alta. (4), Sask. (3), Man. (5), Ont. (2), N.B. (6), N.S. (3), N.L. (2), P.E.I (1), and Yt. (1)
No Activity by 3 Regions:
No Data by 12 Regions:
For more specific information see:
On flu activity: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/fluwatch/2018-2019/week51-52-december-16-december-29-2018.html
Canadian Flu Information:
https://www.canada.ca/en/public-health/services/diseases/flu-influenza.html
General Page for Canadian Flu Watch Surveillance with links to different components:
https://www.canada.ca/en/public-health/services/diseases/flu-influenza/influenza-surveillance.html
About the Canadian Influenza Activity Surveillance System:
https://www.canada.ca/en/public-health/services/diseases/flu-influenza/influenza-surveillance/about-fluwatch.html
Europe:
According to the European Center for Disease Prevention & Control (ECDC), for Week # 52 (Dec 24-30), Influenza activity continued to increase throughout the European Region. Of the samples taken from those with ILI or ARI (acute respiratory illness) by sentinel primary healthcare sites, 37% were positive from flu viruses. The majority of circulating virus remained Influenza A for patients both in hospital and out. In sentinel samples, A (H3N2) and A (H1N1) were about equal in number, while in non-sentinel samples, 2/3 were A (H1N1). Mortality from the 13 Member States reported that all-cause mortality was at expected levels for this time of year.
For more information see: https://flunewseurope.org/
World:
The World Health Organization (WHO) provides info on Influenza in Member Countries here: https://www.who.int/influenza/surveillance_monitoring/en/
First Responder Specific Information
There are many websites that may be helpful in planning and managing seasonal flu within First Responder organizations. A few of those websites are included here:
NIOSH on Flu for Employers/Employees:
https://www.cdc.gov/niosh/topics/flu/
Protection from Flu:
https://www.cdc.gov/flu/protect/habits/index.htm
Weekly Flu Map:
https://www.cdc.gov/flu/weekly/usmap.htm
World Map Showing Flu & Other Infectious Diseases:
https://www.healthmap.org/en/
Other Actions First Responders Should Consider
- First Responders should be vaccinated for Flu each season to prevent getting flu themselves, taking it home to family members, or transmitting it to patients in their care. Family members and patients may be at increased risk of complications from flu.
- Perform proper hand hygiene including frequent handwashing and the use of hand sanitizers in general, and particularly when providing patient care or after touching surfaces.
- Masks (N95 or N100) should be used in the presence of patients with cough and/or fever; preferably before being within 6 feet of the patient. This becomes even more important if droplet producing procedures are being performed (i.e. suctioning, nebulizer treatments, BVM, intubation).
- Care should be taken to avoid touching your own face and mucous membranes (eyes, mouth, nose) since the flu virus is frequently found on surfaces such as door knobs, writing & recording tools (pens and tablets), cot and equipment handles, phones, light switches, as well as clothing, bed clothes, etc.
- Report signs/symptoms of flu to your physician or other appropriate provider for early assessment and care. Alert your employer per policy.
- Cough and sneeze into your sleeve, if a tissue is not available, and not onto your hands. Watch this Youtube video for a humorous but educational approach on the subject. https://www.youtube.com/watch?v=CtnEwvUWDo0
- Stay away from others if you are sick.
- Be aware of your exposure risk and history to prevent exposing others. Take extra precautions or avoid those with immunocompromise, when possible, if you have a known or likely exposure.
- Antivirals may be indicated for the treatment of flu, particularly for those in high risk groups, those who are hospitalized or have severe, complicated or progressing flu. Those that present with 48 hours of the onset of symptoms may also be given antivirals, based on PCP judgement but make sure the practitioner is aware of their Frist Responder Role. See https://www.cdc.gov/flu/antivirals/whatyoushould.htm
And, for consideration when looking at yourself, your family and friends, or your patients, consider the following information regarding complications of flu:
Flu is much more worrisome for the very young and the elderly, as well as those who fit into one of the high risk categories see this link for the list: https://www.cdc.gov/flu/about/disease/high_risk.htm . Signs of ILI/Flu in this group requires careful assessment to rule out complications and these groups are much more likely to need medical oversight to assure adequate care. Young children and those over 65 are typically at greater risk for complications, hospitalization, and even death.
Consideration should be given to perhaps monitoring these groups more closely, with inclination for more comprehensive assessment and transport for further evaluation, when presented with possible flu and any signs of complications.
Complications of flu, sometimes requiring hospitalization and even leading to death, tend to occur after the person has begun to get better from the flu and then appears to relapse. EMS personnel may want to look more closely at those patients when the call is not about the initial signs and symptoms of flu, but about increasing or different signs that have appeared, often from five days to two weeks after the initial flu symptoms began.
A study was published by the Institute for Clinical Evaluative Sciences in NEJM (New England Journal of Medicine). See details below:
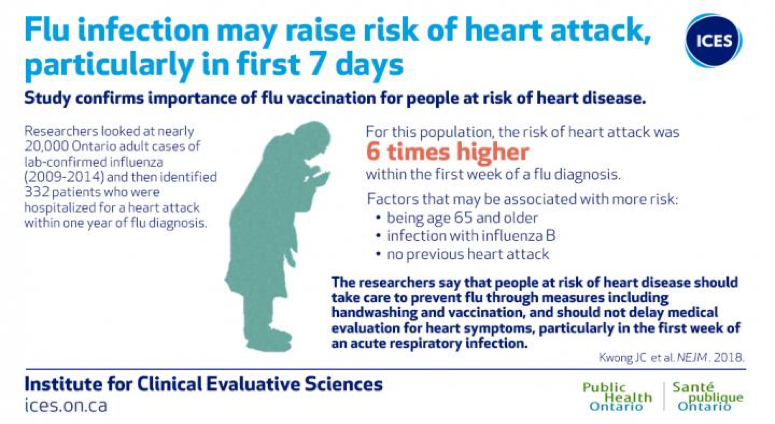
Image courtesy of ICES/PHO
“The researchers add that patients should not delay medical evaluation for heart symptoms particularly within the first week of an acute respiratory infection.” (Lisa Schnirring, News Editor: CIDRAP News ;Jan 25, 2018)
For more information on Influenza and the Heart Attack Study, please see the link below.
https://www.eurekalert.org/pub_releases/2018-01/pho-rcl011818.php

